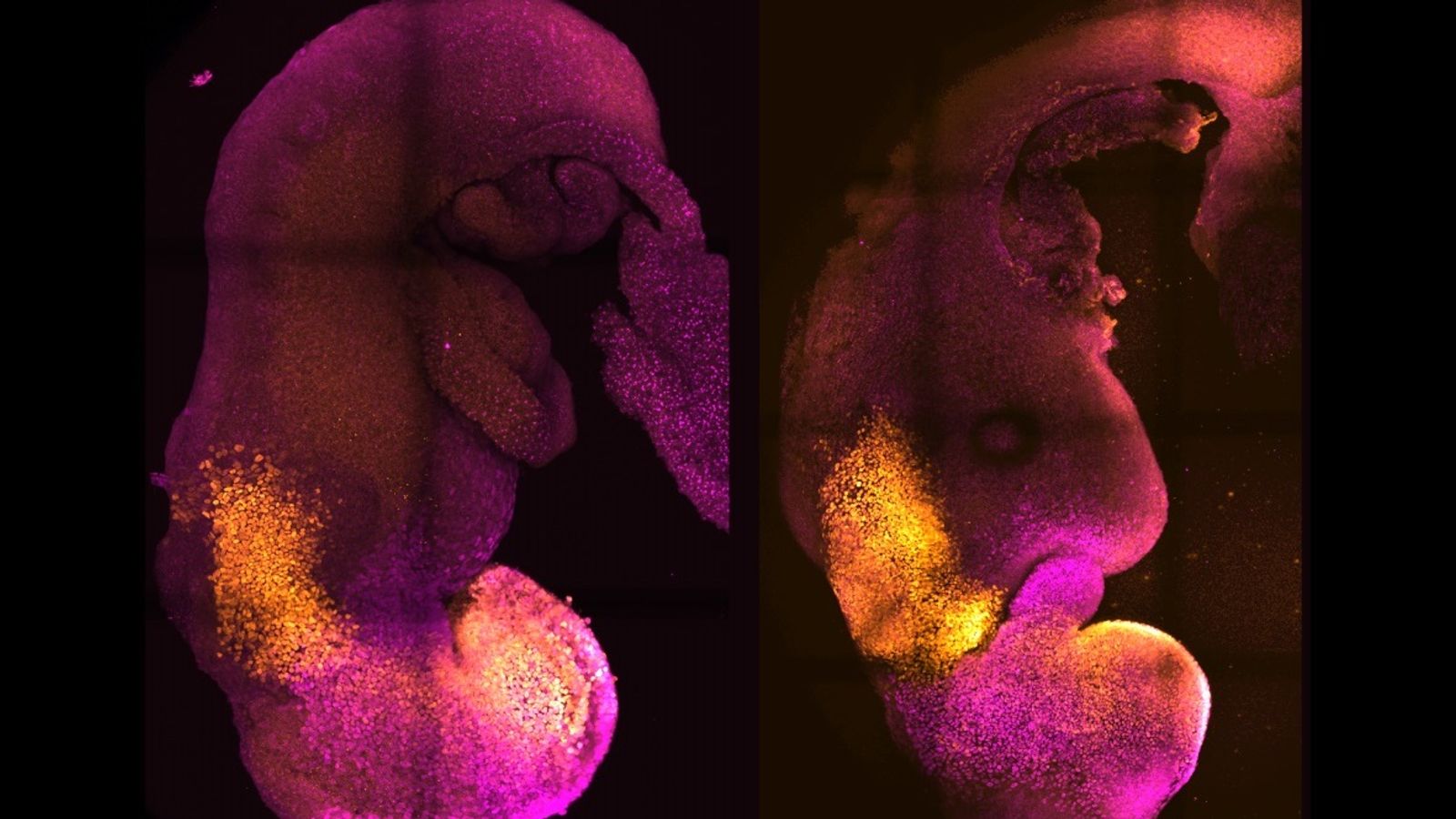
A research team in the UK and US has created “synthetic” mouse embryos that went on to develop a brain, a nerve cord and beating heart tissue in the lab without the need for a fertilised egg or uterus for it to grow in.
It is similar to a breakthrough by an Israeli team, published earlier this month. Together, the breakthroughs promise to revolutionise the understanding of one of biology’s greatest challenges: how a few cells go on to organise themselves into life.
If applied to human embryos, the research could help understand human fertility, developmental disorders and provide a new avenue to develop tissues, or organs, for transplantation grown in the lab.
But applying the technique to human embryos would raise important ethical, and legal questions.
“The big question we’re addressing in the lab is how do we start our lives?” says Professor Magdalena Zernicka-Goetz from Caltech in Pasadena, California, and the University of Cambridge in the UK.
To create synthetic embryos, or “embryoids”, the scientists took three types of stem cell from a mouse embryo which would normally go on to form all the tissues required in a growing embryo.
They then transferred the cells into an artificial growth medium – essentially a rotating flask of nutrients.
Olivia Pratt-Korbel: Police pursuing ‘number of very positive lines of inquiry’ as they hunt gunman
Olivia Pratt-Korbel live updates: Gunman may have fled country, police concede – as second man in gun chase identified
Gary Ballance apologises to Azeem Rafiq for racist language used while playing for Yorkshire County Cricket Club
The stem cells went on to spontaneously form embryos.
Only about one in 100 were successful, but the few that were “are absolutely indistinguishable in many cases from natural embryos” says Prof Zernicka-Goetz.
Read more: New project to unlock the secrets of how human embryos develop
The embryos only developed for eight-and-a-half days, around half-way through the normal gestation period for a mouse.
But the technique should still be hugely important as a way of producing early embryos with which to study early development, without the need for experimental animals.
The team are currently working actively on a human embryo model, but stress it is some way off. There are significant differences between early mouse and early human development.
But having a synthetic human embryo could be a major advance for the study of fertility and common developmental disorders.
“The majority of human pregnancies are lost at the very early stages of our lives,” says Prof Zernicka-Goetz, “and IVF fails in 20 to 70% of cases.”
Supplies of donated human embryos are scarce and often of poor quality, so a lab-grown “model” embryo could help answer many questions.
The team are proposing synthetic embryoids that replicate just one element of an early human embryo, the heart for example, or the tissue that forms the placenta during implantation. Failure at implantation is a major reason for failure of IVF pregnancies.
Synthetic human embryos could also be a way of generating new tissues or organs for “regenerative” medicine. If derived from a patient’s own stem cells such tissues could be a perfect match for the recipient.
However developing synthetic human embryos would, in the UK at least, require a change in the current law which does not cover growing embryos from stem-cells.
UK law also prevents human embryos from being grown in the laboratory past 14 days. This is earlier than most of the important developmental processes seen in these mouse embryos occur.
This latest demonstration means that discussion of these legal and ethical questions should start sooner rather than later, say experts.
“The result does herald that, in the future, similar experiments will be done with human cells and that, at some point, will yield similar results,” says Prof Alfonso Martinez Arias of Universitat Pompeu Fabra in Barcelona who was not connected with the research.
“This should encourage considerations of the ethics and societal impact of these experiments before they happen,” he added.