The World Health Organisation (WHO) has approved a low-cost, readily available vaccine for malaria that promises to help ease one of the greatest disease burdens on the developing world.
The R21 vaccine, developed by the University of Oxford, the Serum Institute of India and drug maker Novavax, could help reduce the 500,000 malaria-associated deaths that occur each year.
It is only the second vaccine to have been approved for the prevention of malaria, after the RTS,S vaccine developed by drug giant GSK was authorised in 2022.
Although the WHO concluded R21 has similar levels of efficacy as RTS,S the new vaccine is expected to be cheaper and should be more widely available.
The Serum Institute of India has production capacity for 100 million doses of R21 each year, which it says will be doubled over the next two years.
Cost and availability are both crucial factors for a vaccine being deployed chiefly in sub-Saharan Africa, where there are nearly 250 million cases of malaria each year.
“The vaccine is easily deployable, cost-effective and affordable, ready for distribution in areas where it is needed most, with the potential to save hundreds of thousands of lives a year,” said Sir Adrian Hill, who led the team developing the vaccine at Oxford University’s Jenner Institute.
The approval of the vaccine follows 30 years of work on malaria at the Jenner Institute. The same lab developed an effective COVID-19 vaccine in less than a year.
But malaria is an altogether tougher challenge.
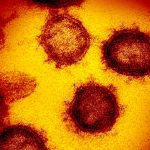
The disease is caused by a protozoan parasite, a single-celled organism with multiple life stages, each evolved to evade the immune response.
The constantly shape-shifting parasite spends much of its life hiding in the liver and red blood cells of its human host, or in the gut and salivary glands of the mosquitoes who transmit malaria.
Compared to some vaccines against infectious diseases like measles or polio, malaria vaccines aren’t good enough to prevent transmission.
In trials, R21 prevented between 68-75% of recipients from contracting malaria. However, in infants – who are most at risk of dying from malaria – levels of protection were between 75-79%.
However, given the fact malaria is such a huge burden and a very difficult target – the WHO set its criteria for an effective vaccine at 75%.
Read more:
US health alert issued after malaria reported in Texas and Florida
Ghana becomes first country to approve Oxford malaria vaccine
“As a malaria researcher, I used to dream of the day we would have a safe and effective vaccine against malaria,” said Dr Tedros Adhanom Ghebreyesus, Director-General of the WHO.
“Now we have two.”
“Demand for the RTS,S vaccine far exceeds supply, so this second vaccine is a vital additional tool to protect more children faster, and to bring us closer to our vision of a malaria-free future,” he added.
The approval of R21 offers additional hope for those working to combat malaria.
Be the first to get Breaking News
Install the Sky News app for free
Between 2000 and 2015, cases and deaths fell significantly due to prevention measures like insecticide-treated bed nets.
Since then, however, progress had been backsliding and WHO was struggling to raise the money needed for its malaria programmes from donor countries.
The rollout of both the RTS,S and R21 vaccines is expected as soon as next year.