There are three main metrics by which the NHS measures its performance in treating cancer – and they are all about how long it takes patients to go through different stages of the health service.
Research by the House of Commons library, commissioned by Labour Shadow Health Secretary Wes Streeting, showed that across all of these measures there are far more people exceeding the targets than there have been historically.
What are the three main metrics?
You are not supposed to wait more than two weeks between seeing your GP and seeing a specialist consultant, at the first stage. If the consultant decides you need treatment, you should have started that treatment within a month after they make that decision.
The third measure checks the whole chain – the time between that first GP referral and the first treatment. Although in theory if you’ve met the other two targets you’ll have been seen in six weeks, the measure gives slightly more leeway – 62 days, so two months.
On the overall 62-day measure, there were about four and a half times more people waiting longer than the target per month from April to November, compared with 10 years ago. On the month-to-treatment measure it’s similar.
For the first measure – the wait between seeing your GP and seeing a cancer specialist has been about 13 times higher.
Because of the often fast-developing nature of cancer, these delays to treatment ultimately mean that many people die who wouldn’t if the NHS was able to treat them as quickly as they were 10 years ago.
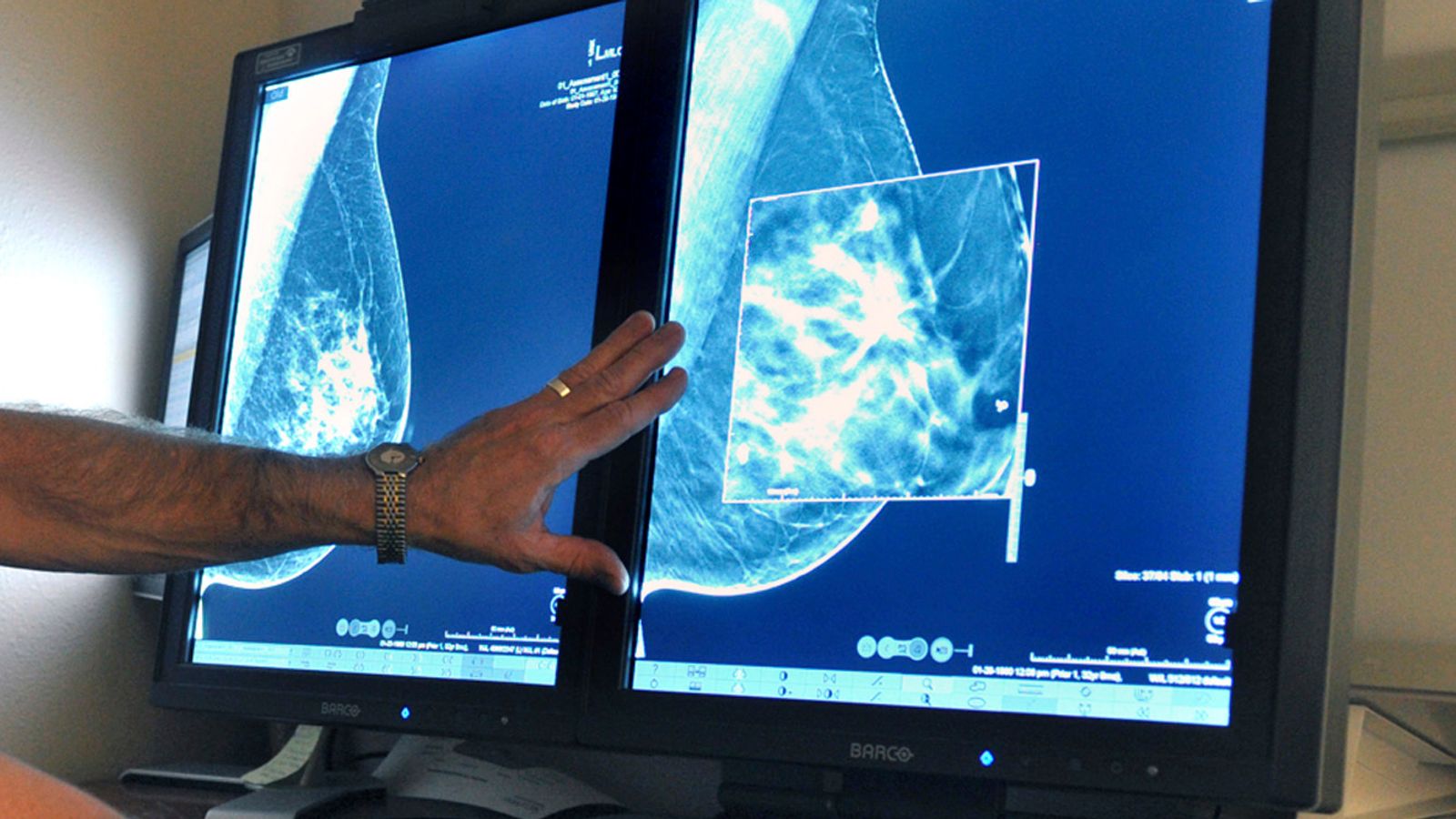
‘Early diagnosis can make a big difference’
“With cancer, early diagnosis can make a big difference when it comes to not only survival chances but treatment options,” explained Tim Gardner, senior policy fellow at the Health Foundation.
“If people have not been able to get care then they may need more invasive and intensive treatments when they’re seen now, which takes longer.”
However, there is more context that needs explaining.
It’s not simply a story of the NHS running out of resources to treat as many people for cancer as it could before.
It is actually treating significantly more people per month than it was 10 years ago.
Let’s look in detail at that key middle measure, the wait for treatment after a specialist has decided you need it.
This chart shows the number of people have had to wait more than a month. It has rocketed up in the last year but was already growing steadily from about 2014, and more steeply since summer 2018.
If we look at that in percentage terms it’s essentially the same story.
However, it’s significant to note that the NHS was failing to reach its target on this measure, consistently over the course of 12 months, before the pandemic started.
So it’s bad news in terms of the real numbers of humans affected and it’s bad in percentage terms as well. But if we look at the other side, the number treated per month, it becomes a bit clearer why that is.
That section at the bottom is the same as the first chart we looked at. It’s also the same as the gap between the other two charts. It has clearly been widening, meaning a smaller percentage of patients are being treated within a month.
But if we look just at the top part of the chart, the NHS is starting cancer treatment for about 7,000 more people every month compared to 10 years ago.
The numbers went down sharply when the pandemic started, and haven’t yet got back up to pre-pandemic levels – staff absences and fatigue will be as much to blame for this as the actual resources taken up treating COVID patients.
At the moment, the numbers of people demanding cancer treatment is exceeding what the NHS can supply.
What about the rest of the NHS?
Cancer waits are often some of the more sensitive measures, but the NHS also collects data on the overall numbers of people waiting for any sort of treatment. It gives a breakdown of how many people have been waiting more than six weeks for certain types of diagnostics tests.
The overall waiting list is also at a record high, almost topping 6 million in November in England alone – more than 10% of the population.
If we look at certain types of treatments, we can see that it’s a slightly different story to cancer.
The waits were getting longer before the pandemic came along. Across all types of tests, the number waiting more than six weeks trebled in 10 years. But we see a huge spike when the pandemic comes along.
Cancer treatment was prioritised during the early stages of lockdown when people were being encouraged to stay away from hospitals and cancel elective operations.
Health experts believe that these missed or cancelled diagnostics tests could be a reason why a lot of people are coming to A&E now in worse condition than we were used to before the pandemic began.
If we look at the number of tests the NHS were doing every month, it dropped sharply and is only now coming back to be at a similar level to before the pandemic for most options.
The waiting times have stayed high though, despite the number of monthly treatments coming back up, because the NHS is still getting through the backlog built up during lockdown.
The Data and Forensics team is a multi-skilled unit dedicated to providing transparent journalism from Sky News. We gather, analyse and visualise data to tell data-driven stories. We combine traditional reporting skills with advanced analysis of satellite images, social media and other open source information. Through multimedia storytelling we aim to better explain the world while also showing how our journalism is done.