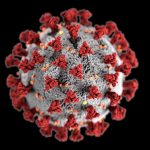
A T cell discovery could lead a development of a vaccine which targets all coronaviruses and COVID variants, a study has suggested.
In a paper published in the Nature journal on Wednesday, researchers said the next generation of COVID vaccines should aim for the body to respond to specific proteins that are essential for the virus’s earliest stages.
By designing jabs that activate immune memory cells – known as T cells – to attack infected cells, it may be possible to eliminate COVID at the start and help to stop its spread, the study suggested.
Live COVID updates from the UK and around the world
This could complement COVID-19 vaccines currently licensed in the UK, which only trigger immune responses to the spike protein that protrudes from the outside of the virus.
Researchers said the discovery could lead to the creation of a vaccine for all coronaviruses, which would not only protect against COVID and its variants, but also against coronaviruses that cause common colds and new emerging animal coronaviruses.
COVID-19: Antibiotic use decreased during first year of pandemic, research suggests
Patients with serious conditions ‘at risk’ due to record ambulance delays, paramedics warn
Thousands of care home staff to lose their jobs as mandatory COVID-19 vaccine deadline passes
Senior author Professor Mala Maini, of University College London’s (UCL) Division of Infection & Immunity, said: “Our research shows that individuals who naturally resisted detectable Sars-CoV-2 infection generated memory T cells that target infected cells expressing the replication proteins, part of the virus’s internal machinery.
“These proteins – required for the earliest stage of the virus’s life cycle, as soon as it enters a cell – are common to all coronaviruses and remain ‘highly conserved’, so are unlikely to change or mutate.
“A vaccine that can induce T cells to recognise and target infected cells expressing these proteins, essential to the virus’s success, would be more effective at eliminating early Sars-CoV-2, and may have the added benefit that they also recognise other coronaviruses that currently infect humans or that could in the future.
Please use Chrome browser for a more accessible video player
“T cells recognising the virus’s replication machinery would provide an additional layer of protection to that provided by the spike-focused immunity that is generated by the already highly efficacious current vaccines.
“This dual-action vaccine would provide more flexibility against mutations, and because T cells can be incredibly long-lived, could also provide longer-lasting immunity.
“By expanding pre-existing T cells, such vaccines could help to stop the virus in its tracks at a very early stage.”
A UCL and St Bartholomew’s Hospital-led observational study, COVIDsortium, analysed the immune responses of London-based healthcare workers from the start of the first wave of the pandemic in the UK.
In a subset of healthcare workers who showed no sign of COVID infection – repeatedly testing negative – there was an increase in T cells.
Rather than having avoided infection completely, a subset of healthcare workers appear to have experienced a transient low-level (abortive) infection, not detectable by routine tests.
But it generated T cells specific to COVID – compatible with this, the same individuals also had a low-level increase in another blood marker of viral infection.
Lead author, Dr Leo Swadling, of UCL’s Division of Infection & Immunity, said: “We know that some individuals remain uninfected despite having likely exposure to the virus.
“What we didn’t know is whether these individuals really did manage to completely avoid the virus or whether they naturally cleared the virus before it was detectable by routine tests.
“By intensively monitoring healthcare workers for signs of infection and immune responses, we identified a minority with this particular SARS-CoV-2 specific T cell response.
Follow the Daily podcast on Apple Podcasts, Google Podcasts, Spotify, Spreaker
“What is really informative is that the T cells detected in these individuals, where the virus failed to establish a successful infection, preferentially target different regions of the virus to those seen after infection.”
Commenting on why some people might be able to clear an infection better than others, he added: “It could be due to the infection history of these individuals.
“The healthcare workers that were able to control the virus before it was detectable were more likely to have these T cells that recognise the internal machinery before the start of the pandemic.
“These pre-existing T cells are poised ready to recognise Sars-CoV-2.”